Photo by Alexander Grey/Unsplash.
Long COVID could be caused by the virus lingering
in the body. Here’s what the science says:
by Stephen Kent, The University of Melbourne and Chansavath Phetsouphanh, UNSW Sydney
While most people survive and recover from COVID, for some people symptoms can persist for months or years. When symptoms last longer than 12 weeks, the condition is known as long COVID.
Long COVID encompasses up to 200 different symptoms. To determine evidence-based treatments for these symptoms, we need to understand the causes. One factor that may be associated with long COVID is that the virus hasn’t fully cleared from the body after the initial infection.
We know from other viruses that viral fragments can remain in different tissues for months or even years. This could be the case with SARS-CoV-2, the virus that causes COVID. Here’s what the science says so far.
Other viruses lurk in the body
Herpesviruses (such as Epstein-Barr virus, the cause of glandular fever), as well as HIV (human immunodeficiency virus) can exist in a “latency state” for life. This means the virus conceals itself within cells and remains dormant.
HIV, in particular, can remain dormant in infected cells throughout the body. Even though it’s inactive, it can still promote immune activation and inflammation.
Other viruses such as Zika, measles and Ebola have been found in tissues of infected people months or years after initial infection. This viral persistence can cause chronic illness.
Several studies have shown COVID can also reactivate the Epstein-Barr virus, which has remained in the body in a latent state. Research shows this has been linked to fatigue and problems with thinking and reasoning in people with long COVID.
 Latent viruses can cause fatigue and problems with thinking and reasoning. Wes Hicks/Unsplash
Latent viruses can cause fatigue and problems with thinking and reasoning. Wes Hicks/Unsplash
How do we know COVID stays in the body?
Several studies have identified the genetic sequences of SARS-CoV-2 (RNA) as well as SARS-CoV-2 proteins in tissues and stool (poo) samples months following infection.
These studies include multiple autopsy reports that found viral RNA and protein in a variety of tissues from people who died up to seven months after infection. SARS-CoV-2 RNA was detected in at least half the samples of heart, lymph glands, eye, nerve, brain and lung tissue tested.
In people who survived, viral RNA was found four months after infection within intestinal tissues obtained through colonoscopy, when a thin tube is used to take tissue from the large intestine. These patients had asymptomatic COVID and were PCR-negative from swabs of the nose and throat at four months.
A 2022 study found SARS-CoV-2 in the stool of about half of the participants in the first week after infection. At four months, there was no virus present in the respiratory tract but 12.7% of stool samples were RNA positive. A further 3.8% of faecal samples remained positive for RNA at seven months.
Initial studies did not always suggest a strong relationship between the long-term detection of SARS-CoV-2 and long COVID symptoms.
But more recently, the presence of SARS-CoV-2 RNA (or protein translated from RNA) in the blood and gut tissue was found to increase the likelihood of developing long COVID symptoms.

The presence of SARS-CoV-2 in the blood increases the likelihood of developing long COVID symptoms. Photo by Nguyễn Hiệp/Unsplash
How might the delay in clearing the virus impact people with long COVID?
Delayed clearance of SARS-CoV-2 particles in different parts of the body could drive illness through several potential processes:
1) Inflammation. The continued immune stimulation by viral proteins causes inflammation, makes our immune system tired, and alters how our immune cells work as time goes on.
We have previously shown immune dysfunction and inflammation persist up to eight months in people with long COVID that initially had mild to moderate disease.
2) Activation of other dormant viruses. The continued immune response to persistent SARS-CoV-2 can cause reactivation of latent viruses.
Antibodies reactive to Epstein-Barr virus are elevated in people with long COVID suggesting Epstein-Barr virus reactivation, likely through activating the immune system.
Other latent viruses, such as human endogenous retroviruses (HERVs; ancient viruses that have become a part of our DNA, like a genetic fossil) have recently been shown to become reactivated after infection. HERV proteins were detected in blood cells and tissues of COVID patients.
These proteins could potentially drive inflammatory processes in long COVID.
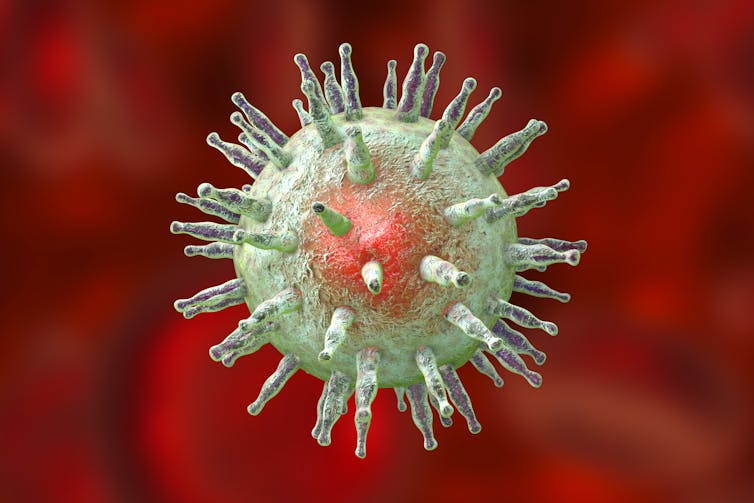
Reactivation of the Epstein-Barr virus could drive inflammation in long COVID. Shutterstock
3) Antibodies made by combating SARS-CoV-2 could become “self” reactive. These autoantibodies (antibodies produced by our immune system that mistakenly target and attack our own body’s tissues or organs) might cross-react with host receptors or proteins and drive autoimmune disease.
Importantly, recent studies have shown new onset of autoimmune diseases (such as type 1 diabetes, inflammatory bowel disease and psoriasis) are significantly associated with SARS-CoV-2 infection and a link between autoimmunity and long COVID is plausible.
This suggests COVID not only has immediate health impacts but could also potentially trigger long-term changes in the immune system.
While the studies mentioned above provide initial evidence of persistence of SARS-CoV-2 long after initial infection, more studies are needed to show a convincing link between lingering virus and long COVID. This should include examination of viral RNA and protein in both blood and tissues in people with long COVID independent of disease severity. And it must involve well-developed cohort studies that track large groups of people internationally.
Several trials are underway to assess whether treating long COVID with antivirals such as Paxlovid may reduce viral antigens and improve symptoms, although this remains experimental.![]()
Stephen Kent, Professor and Laboratory Head, The University of Melbourne and Chansavath Phetsouphanh, Senior Research Associate, Kirby Institute, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Contact us by email at fund4thepanamanews@gmail.com
To fend off hackers, organized trolls and other online vandalism, our website comments feature is switched off. Instead, come to our Facebook page to join in the discussion.
These links are interactive — click on the boxes